A book is written together by the National research Council, the Committee on the main challenge areas for convergence and health, the Division on Earth and life studies and the Board on life sciences describe the convergence of health and other disciplines as follows: “Convergence of the life sciences with fields including physical, chemical, mathematical, computational, engineering, and social sciences is a key strategy to tackle complex challenges and achieve new and innovative solutions. However, institutions face a lack of guidance on how to establish effective programs, what challenges they are likely to encounter, and what strategies other organizations have used to address the issues that arise. This advice is needed to harness the excitement generated by the concept of convergence and channel it into the policies, structures, and networks that will enable it to realize its goals.”[1]. This statement summarizes the necessity, and challenges of convergence and the requirement of new policies. In fact, there two different sides of the convergence of digital health technologies and health policy. 1) The challenges brought about by the convergence of health care and digital health technologies require the development of different public health systems to protect public from their harmful effects, and 2) Digital health technologies and health care disciplines can be used to develop health policies to enhance public health care. Convergence of healthIT, public policy and medicine is illustrated in Figure 1.
Figure 1. Convergence of preventive health care, Digital health technologies, and public health policy
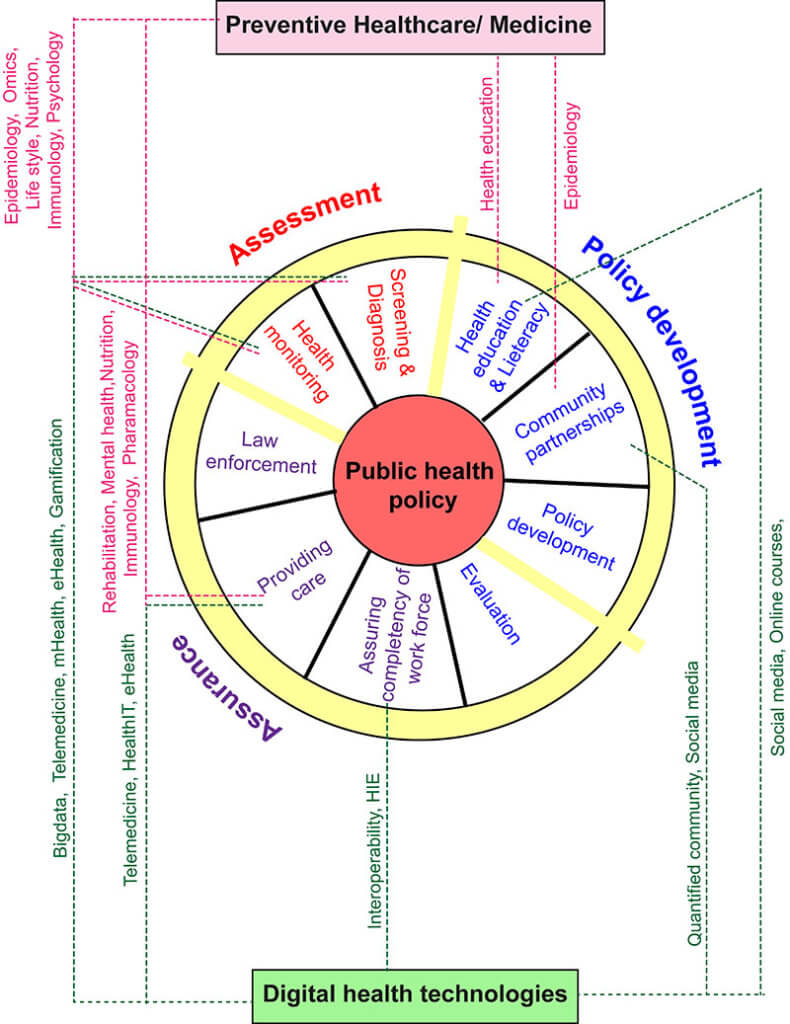
The panel on the goals of health plans was adapted and modified from [2].
According to a model from CDC, public health policy and associated health status development are composed of three essential services 1) Assessment, 2) Policy development and 3) assurance [2]. The involvement of preventive health care themes and digital health technologies in many of these services are outlined in Figure 1. This one side of the convergence where advances in preventive health care and digital health technologies aid the development of different health policies.
| Recommended for you | |
| Convergence of preventive health care themes | |
| Role of policy in guiding digital health revolution | |
| 10 Digital health technologies empowering patients |
Health convergence and change in health care model
This convergence came equipped with its challenges and weakness required not only different health plans but an overall makeover in traditional biomedical health care model. This interdisciplinary model of health care has driven academics, researchers and health professionals to explore novel avenues and also come with solutions for health issues that can not be solved by traditional approaches which may require breaking or ending the currently available boundaries between disciplines [3]. And this amendment to the current limits requires a development of new public health policies. The ‘novel interdisciplinary model of converged health care’ needs multi-agency initiatives for regulating, funding and managing collaborations between disciplines[4]. Moreover, this original model provides an excellent ground for research [4].
One of the challenges in the current health care system, as seen by many medical professionals, is that the health systems in many places are overwhelmed due to high caseloads, low efficiency and many of the patients have to seek medical support from community health care [5]. In such cases, some of the health care institutions accept low-quality health policies that may not be up to the standards. Incorporation of digital health technologies such as Telemedicine, remote monitoring, and HIE will immensely facilitate patient treatment outcomes if proper financial and technological support along with ‘universal health care policies’ or ‘international health care policies’ are provided to these places[5].
For this novel interdisciplinary health care model to function effectively regardless of the distance between the patient and the health care provider, the exchange of health information has to be carried out efficiently. However, the current Health Insurance Portability and Accountability Act (HIPAA) acts as a barrier for such data exchange [6]. While the current health policies attempt to protect the privacy and safety of the patients by doing so, they do act as barriers in the different health care model. For the health professionals to share HER through HIE, they should be provided with necessary education regarding disclosure of protected health information in public health use which includes health monitoring, diagnosis, interventions and treatment [7].
HealthIT cybersecurity, ransomware and health policies
With the involvement of digital IT technologies in healthcare settings, as usual to any IT-related field, there emerged the risk of patient and medical information being hacked and misused. This has led to the implementation of ‘HealthIT cybersecurity’ and health policies associated with it. For instance, mental health data breach can be of the critical national security issue and thus emphasizes the necessity to comply with HIPAA regulations when maintaining, transferring, and sharing mental health data[8]. For this reason, many healthcare and associated institutions and companies pay much attention in controlling HealthIT cyber security by implementing and maintaining data encryption, configuration management and risk assessment [9].
Interoperability and health policies
Interoperability is an essential component of the interdisciplinary healthcare model. In 2009, the Health Information Technology for Economic and Clinical Health (HITECH) Act was established to regulate the health data/information exchange between health care professionals and outside parties such as ambulatory care, pharmacy, and healthcare institutions involved in telemedicine [10, 11]. The fundamental goal of HITECH Act is to “promote the adoption and meaningful use of health information technology” [10]. To resolve the lack of interoperability in many of the healthcare partners, the Agency for Healthcare Research and Quality and the President’s Council of Advisors on Science and Technology (PCAST) issued many recommendations in 2014, enabling these healthcare partners to enhance their interoperability infrastructure [11]. They also attempt to implement a ‘universal exchange language’[11].
Image credit: www.istockphoto.com